- Review
- Open access
- Published:
Occupational, environmental, and toxicological health risks of mining metals for lithium-ion batteries: a narrative review of the Pubmed database
Journal of Occupational Medicine and Toxicology volume 19, Article number: 35 (2024)
Abstract
Background
The global market for lithium-ion batteries (LIBs) is growing exponentially, resulting in an increase in mining activities for the metals needed for manufacturing LIBs. Cobalt, lithium, manganese, and nickel are four of the metals most used in the construction of LIBs, and each has known toxicological risks associated with exposure. Mining for these metals poses potential human health risks via occupational and environmental exposures; however, there is a paucity of data surrounding the risks of increasing mining activity. The objective of this review was to characterize these risks.
Methods
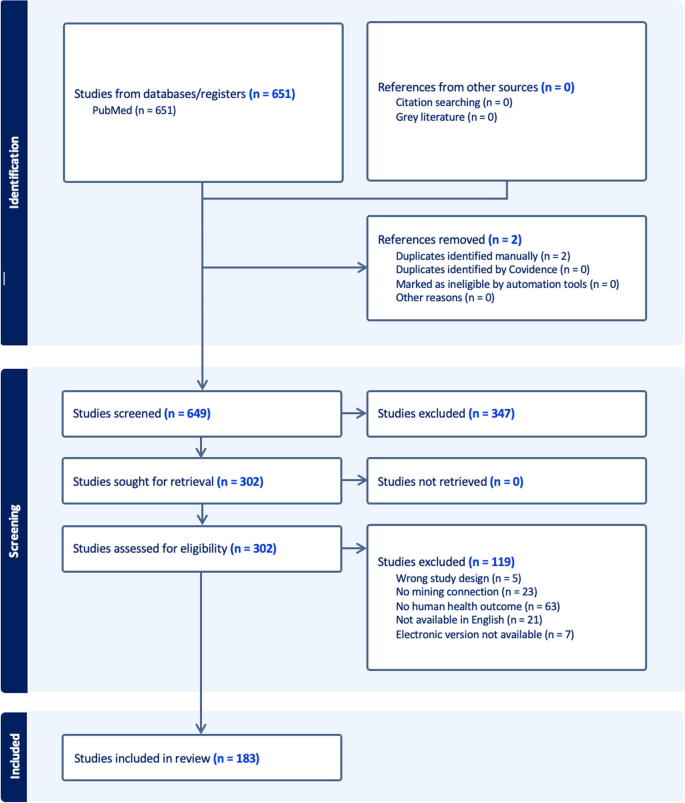
We conducted a review of the literature via a systematic search of the PubMed database on the health effects of mining for cobalt, lithium, manganese, and nickel. We included articles that (1) reported original research, (2) reported outcomes directly related to human health, (3) assessed exposure to mining for cobalt, lithium, manganese, or nickel, and (4) had an available English translation. We excluded all other articles. Our search identified 183 relevant articles.
Results
Toxicological hazards were reported in 110 studies. Exposure to cobalt and nickel mining were most associated with respiratory toxicity, while exposure to manganese mining was most associated with neurologic toxicity. Notably, no articles were identified that assessed lithium toxicity associated with mining exposure. Traumatic hazards were reported in six studies. Three articles reported infectious disease hazards, while six studies reported effects on mental health. Several studies reported increased health risks in children compared to adults.
Conclusions
The results of this review suggest that occupational and environmental exposure to mining metals used in LIBs presents significant risks to human health that result in both acute and chronic toxicities. Further research is needed to better characterize these risks, particularly regarding lithium mining.
Introduction
In recent years, the global market for lithium-ion batteries (LIBs) has grown exponentially in response to increasing economic and political interests in energy alternatives to fossil fuels [1]. LIBs are rechargeable batteries that are used in a multitude of products including electric motor vehicles, smartphones, laptops, power tools, and energy storage systems. Rapid economic growth is projected to continue, with the global LIB market currently valued around $54 billion and anticipated to increase by 20–30% annually until 2030 [2, 3]. Consequently, there has been a dramatic increase in efforts to mine the metals used to manufacture LIBs [4].
In addition to the titular lithium, LIBs contain transition metals that are typically used to construct the cathode of the battery system [5]. The anode is generally constructed of graphite. Cobalt, manganese, nickel, and lithium are four of the most heavily mined metals for LIB production [5]. Large quantities of these metals are often required for manufacturing. A single car battery, for example, can contain up to 20 kg of cobalt [6]. Significant expansion of mining activities for these metals is occurring on a global scale and poses potential health risks to mine workers and neighboring communities via occupational and environmental exposures [7]. Despite this, there is a paucity of data surrounding the risks of such increased mining activity.
Each of the metals in this study has well-documented toxicity. The respiratory effects of cobalt have been described for centuries, since German miners discovered that toxic gases were released during the smelting process [8]. The miners believed the metal was bewitched by devilish spirits and nicknamed the metal “kobold” or “goblin of the mines”. Cobalt inhalation can cause direct respiratory toxicity, including hard metal lung disease, while systemic cobalt toxicity can cause cardiomyopathy, thyroid dysfunction, neurologic dysfunction, and aseptic lymphocyte-dominated vasculitis-associated lesions [9]. The neurotoxicity of manganese has been extensively documented and was described as early as the nineteenth century. Occupational and environmental exposures have been associated with numerous neurologic and psychiatric manifestations including Parkinsonism, motor deficits, cognitive impairment, and psychosis [10]. Nickel is a known genotoxin and carcinogen [11]. Occupational exposure primarily occurs through inhalation; however, toxicity can also develop via ingestion or skin absorption [12]. Lithium is nephrotoxic and thyrotoxic, can cause neuropsychiatric symptoms, and is a teratogen [13, 14].
In this study, we conducted a narrative review of the occupational, environmental, and toxicological hazards associated with mining exposure to cobalt, lithium, manganese, and nickel to better characterize the risks associated with growing demand for LIBs.
Methods
We systematically searched the PubMed database using the pre-defined search term “((cobalt) OR (lithium) OR (manganese) OR (nickel)) AND ((health) OR (disease) OR (injury)) AND ((mine) OR (mining))” on January 24, 2024. We analyzed the results of the search in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. We did not apply any other restrictions to the initial search. We imported all studies resulting from this search into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) for review. A minimum of two authors independently screened titles and abstracts for inclusion, with discrepancies resolved by a third author. We then reviewed full texts for all articles included in the screening.
We included studies if they (1) reported original research, (2) reported outcomes directly related to human health, (3) assessed exposure to mining for cobalt, lithium, manganese, or nickel, and (4) had an English translation that could be obtained electronically either via internet search or inter-library loan. We excluded studies that did not meet all inclusion criteria. Following review, we extracted the following variables from the articles meeting inclusion criteria, as applicable: date of publication, country or countries in which the study was conducted, study design, which of the four previously chosen metals (cobalt, lithium, manganese, or nickel) were included, report of human health or toxicological hazards, report of traumatic hazards, report of non-traumatic occupational hazards, and calculated health risk based on environmental data.
Results
The initial search term yielded 649 unique articles, of which 183 met inclusion criteria (Fig. 1). The final set of included articles contained 22 cohort studies, 3 case–control studies, 91 cross-sectional studies, and 4 case reports or series, in addition to 2 in vitro studies and 61 articles that calculated human health risk based on environmental sampling without including human participants. Included articles were published between 1955 and 2023 and came from 47 countries (Fig. 2). The countries that appeared most frequently were China (30 articles), the Democratic Republic of the Congo (12), Mexico (11), and South Africa (11). Manganese appeared in the most articles, while lithium appeared in the least. Many articles discussed more than one of the study metals.
Toxicological hazards: cobalt mining
Toxicity associated with exposure to cobalt mining was assessed in 28 articles [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. Respiratory disease was the most common category of toxicological hazard reported in papers discussing cobalt exposure. Respiratory health problems described in populations exposed to cobalt mining included upper and lower respiratory infections, lung cancer, hard metal lung disease, pneumoconiosis, chronic bronchitis, and chronic mountain or altitude sickness [24, 25, 29, 39, 40, 42]. A case report discussed a patient in whom hard metal lung disease re-occurred even after a lung transplant [42]. Three studies conducted in areas of the Democratic Republic of the Congo known for cobalt mining described birth defects in children whose parents held mining-related jobs [26, 27, 43]. Several studies reported increased in vivo levels of heavy metals in populations exposed to mining compared to reference values or control groups [17, 18, 20, 22, 32, 36, 37]. Levels as much as 40 times greater than reference values were reported [17]. One such study also found that exposed children had higher urine levels of DNA oxidative damage markers, a difference that was not observed in adult participants [18]. In pregnant women exposed to cobalt mining, elevated maternal blood levels were associated with fetal levels, suggesting cross-placental transfer [28]. Cobalt mining work was also reported to be associated with male sexual dysfunction and decreased testosterone [33, 34].
Toxicological hazards: manganese mining
Toxicity associated with exposure to manganese mining was assessed in 73 papers, more than any other metal in this study [16,17,18,19,20,21, 23, 31, 32, 35, 37, 38, 41, 43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102]. Neurologic toxicity was the most cited category of disease, with studies reporting cognitive impairment, muscle weakness, gait instability, tremors, impaired motor control, hearing loss, memory problems, and Parkinsonism [46, 58, 61, 66, 68, 71, 89,90,91,92]. Psychiatric symptoms were described in multiple studies including higher scores on psychiatric distress assessments, emotional instability, disorganization, manic symptoms, and hallucinations [44, 89, 92]. Increased iron deficiency among manganese miners was reported in one study and rates of iron deficiency improved after reconstitution of drinking water [48]. Manganese mining exposure was also associated with prostate cancer, prolactin levels, and sexual dysfunction [81, 89, 92, 96, 99]. Respiratory disease was less commonly reported in papers discussing manganese mining than for cobalt or nickel, although studies did report associations between exposure to mining activities involving manganese and worse respiratory function metrics, pneumoconiosis, respiratory infections, and development of restrictive lung disease [47, 70, 89, 94]. Cytotoxic and immunotoxic effects in mining-exposed populations were described in multiple studies, including T-cell receptor mutations, and lower levels of CD3 + and CD4 + lymphocytes [55, 56]. In one in vitro study, exposure to manganese oxides obtained from mine dust was associated with DNA damage [45]. Multiple studies assessed risks in children. Studies reported that the concentration of manganese in the hair of children living near mines was elevated compared to controls and associated with worse performance on visuospatial and verbal learning and memory testing [63, 66]. Manganese in umbilical cord blood was reported to be associated with birth defects in a case–control study while cognitive and motor function in children was negatively associated with maternal levels of manganese [43, 54]. A study comparing children living in a manganese mining area to a control group found decreased performance on IQ testing [88]. Children exposed to manganese mining were also reported to have higher incidence of skeletal deformities [62]. Increased in vivo levels of manganese associated with mining exposure were also described in several studies [16, 20, 35, 38, 47, 48, 65, 66, 69, 84, 88, 93].
Toxicological hazards: nickel mining
Toxicity associated with exposure to nickel mining was assessed in 56 papers [17, 20, 21, 23, 31, 32, 35, 37,38,39, 41, 45, 55, 56, 60, 67, 77, 83, 87, 97, 102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137]. Like cobalt, respiratory toxicity was the most common type of pathology reported. Respiratory manifestations associated with nickel mining included lung cancer, chronic bronchitis, respiratory infections, and nasal obstruction/rhinitis [39, 109,110,111, 118, 119, 123, 128, 133]. Increased mortality due to other types of cancer and cardiovascular disease was also reported in populations exposed to nickel mining and refining.120,125 One study found that 75% of participants living in a nickel mining region who used dug wells as a water source had elevated urinary creatinine [131]. Mine workers exposed to nickel were found to have higher urinary nickel and cystatin C levels than steel plant workers [135]. A large cross-sectional study found increased diabetes in nickel miners compared to office workers [136]. Constitutional growth delay was reported at several times greater prevalence in a population exposed to manganese and nickel pollution relative to a control population [102]. Studies also reported elevated markers of DNA damage, inflammatory markers, and auto-antibodies among populations exposed to nickel mining [105, 108, 112, 122]. DNA damage was also shown to be induced by in vitro exposure to mine evaporite [124]. Populations exposed to mining were found to have elevated nickel levels in blood, urine, hair, and breast milk compared to reference values or control groups [20,21,22, 31, 32, 37, 41, 60, 77, 97]. Elevated physiologic levels were observed multiple decades after the cessation of mining activity, indicating the longevity of environmental contamination [107].
Toxicological hazards: lithium mining
No studies identified in this review described toxicological effects associated with lithium exposure due to mining.
Infectious disease hazards
Infectious disease hazards were described in three articles. Two studies reported outcomes from a Histoplasmosis outbreak among manganese mine workers in Guyana in 2019 [98, 100]. The third study was a survey conducted in a South African mining community, in which miners expressed concerns regarding high rates of communicable diseases, including tuberculosis and HIV. The miners cited residential overcrowding, inadequate toilet facilities, and prostitution as contributing factors [86].
Traumatic/physical hazards
Six articles were found that reported traumatic injuries or fatalities associated with mine work. Studies reported a variety of traumatic hazards, including falls, cave-ins, explosions, and mine fires [95, 117, 138] These hazards were reported to be associated with the quality of working conditions and factors such as poor visibility, extreme noise, and inadequate ventilation. Injuries related to machinery were cited in multiple studies and attributed to both inadequate training and malfunctioning or outdated equipment. Interviews with manganese miners reported insufficient personal protective equipment as a hazard and described a culture in which reluctance to work in unsafe conditions is penalized by supervisors, potentially resulting in job loss [86]. Two large retrospective studies of mortality among Canadian nickel workers found significantly increased mortality due to injury or violence compared to expected values [104, 127]. Although these studies did not differentiate between fatal injuries that occurred in occupational versus non-occupational settings, injury mortality was particularly increased among underground miners.
Psychiatric/mental health hazards
Psychiatric illness and effects on mental health were reported in six papers. Chronic stress was described in multiple papers and occupational stress was associated with worse perceived quality of life [86, 121]. Higher scores on a standardized survey of psychological distress were recorded among participants residing in areas with increased levels of metal contamination [44]. An early study of mine workers with manganese poisoning described multiple psychiatric symptoms including mood instability and psychosis [92]. A survey of over 1000 nickel miners in China reported symptoms of burnout in more than 80% of participants [130]. Increased mortality due to suicide was also reported among miners [104].
Environmental sampling
A total of 61 studies measured levels of metals in environmental samples from areas contaminated by mining activity and calculated health risk via pre-determined acceptable values [139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199]. These studies did not directly involve human participants. A variety of substrates were sampled including soil, water, air, plants, and animal tissue. Non-carcinogenic health risks were reported in many studies and determined from the Total Hazard Quotient or Hazard Index. A smaller subset of studies also reported carcinogenic risks, which were calculated based on standardized cancer slope factors and compared to acceptable levels determined by the International Agency for Research on Cancer. Of the studies, 43 reported a Hazard Index > 1 or lifetime cancer risk > 1 × 10–4 for one or multiple metals in at least one assay, indicating unacceptable levels of risk. In 14 of these studies, reported risks were increased for children compared to adults.
Discussion
The results of this literature review demonstrate the breadth of adverse outcomes on health and wellbeing associated with occupational and environmental exposure via mining to the four metals historically most used in the construction of LIBs. Our results are largely consistent with known pathologic mechanisms; cobalt and nickel mining were more commonly discussed in articles describing respiratory disease, while all studies reporting neurologic pathology involved manganese exposure. Given the exponential growth of mining for these metals in recent years, it is likely that effects on human health will increase without mitigation efforts.
The lack of studies examining the health effects of lithium mining is noteworthy given the recent exponential increase in the global market for this metal, which has been termed “white gold”. Pathologic manifestations of both acute and chronic lithium toxicity have long been recognized medically given its common use as a treatment for psychiatric illness and its narrow therapeutic index. Less is known about the effects of environmental lithium, although studies have reported associations between naturally occurring lithium concentrations in ground water and psychiatric illness, thyroid dysfunction, and adverse birth outcomes [200,201,202]. Lithium mining has also been shown to increase the concentration of other heavy metals, such as arsenic, in surrounding surface water [203]. In traditional lithium mining, salt-rich brine is pumped from deep in the earth to the surface, forming man-made lakes that are then allowed to evaporate [204]. Lithium can also be mined from hard rock ores. Given the methods used in lithium mining, it is reasonable to hypothesize that there is a significant risk of environmental contamination, which might lead to toxicity from lithium and other metals. Additional chemicals are often added to the brine to facilitate the precipitation of unwanted compounds. Multiple instances of lithium mining affecting nearby communities have attracted media attention, such as the 2016 contamination of the Liqi River in Tibet resulting in the destruction of the local water supply and the death of livestock and fish used as a food source [205]. Despite these high-profile incidents, no studies could be found examining the health effects of exposure to lithium mining.
Our review revealed other concerning gaps in the literature, specifically a paucity of studies describing infectious and traumatic hazards. Mine workers often reside in overcrowded conditions with poor sanitation, infrastructure, and inadequate access to medical care. These conditions promote the transmission of communicable diseases such as malaria and tuberculosis [206]. In addition, the construction of mining facilities often encroaches on the natural habitats of wild animals that may expose workers to zoonotic pathogens [207]. Sexually transmitted diseases including HIV are also prevalent in many mining communities, which can be sites of prostitution and sex trafficking [32, 208, 209] Similarly, few articles discussed traumatic and violent injuries, even though it is well known that many miners work in unsafe conditions and are subjected to falls, cave-ins, injuries from machinery, and other hazards [210]. Traumatic hazards arise from the essentially dangerous nature of mining work and are often compounded by a lack of safety regulations and cultural and economic systems that incentivize workers to perform unsafe tasks.
There are multiple likely explanations for this lack of data. The populations most affected by mining activities are inherently vulnerable. They are often poor, and many are migrants. In some countries, they are subject to human rights violations [209]. People depend on the mines as a source of income and may therefore be less likely to engage with researchers or report accidents for fear of retribution or loss of employment. This can be compounded by the fact that small-scale mining practices are often carried out in violation of local laws. Additionally, access to healthcare is inadequate in many areas, and health systems that do exist may lack the ability to track and report outcomes. Further research and illumination of the plight of miners may also represent a conflict of interest with mining companies that benefit from a source of cheap, exploitable labor. The logistics of carrying out studies are therefore more difficult.
In response to these issues, some mining areas have implemented environmental management programs (EMP) aimed at mitigating the exposure to these metals in mining communities [48, 57, 58]. The strategies utilized by these EMPs are aimed at decreasing dust emissions to decrease the particulate matter in the air. This includes improving clean water availability; updating to equipment that decreases emissions; paving roads and frequently travelled routes; and reforesting the areas. Studies have shown EMPs in manganese mining communities decreased the air concentration of manganese; however there have been variable results regarding the effect on health outcomes [57, 58]. Nevertheless, EMPs are an important step in decreasing the health risks. Other potential interventions to help mitigate health risks include increasing the use and availability of personal protection equipment as well as implementing a medical surveillance program to monitor exposures [48].
An interesting subset of studies in this review collected qualitative information via interviews that present the perspectives of people who work in and live near mining sites [32, 49,50,51,52, 86, 109,110,111, 117]. Overall, there is evidence that affected populations are aware that mining poses significant health risks; however, there is economic and social pressure to tolerate health hazards to make a living. Participants reported that engaging in protests or voicing opposition to mining development placed them at risk of violent suppression from police or military forces or ostracization from other members of the community. In interviews, people living near the mines reported a perceived connection between the growth of mining activities and various health problems including acute and chronic symptoms (e.g., respiratory illnesses, chest pain, chronic headaches), impaired cognitive development in children, pollution of air and water, and destruction of farmland. Displacement of local populations by expansion of mining sites was also reported. These studies highlight the complex effects, both positive and negative, of mining presence in a community.
The results of this review are consistent with well-documented prior data suggesting that children are at disproportionately increased risk from metal toxicity compared to adults [211,212,213]. Children are at increased risk for toxicity due to heavy metal exposure for multiple reasons including their smaller body size, tendency to ingest non-food materials, hand-to-mouth behaviors, and the increased risks of exposure during physiologic and cognitive developmental periods. Multiple studies in our review reported increased adverse health outcomes in children relative to adults in the same populations [17, 18, 32, 40, 41, 76]. Child labor is also unfortunately common in many mining industries. An estimated 40,000 children work in cobalt mines in the Democratic Republic of Congo [7]. In addition to the physical hazards associated with mine work, they also face the consequences of lost years of education and mental health trauma.
A significant number of studies in this review focused on measuring levels of metals in environmental substrates such as soil, water, plant, and animal specimens to calculate estimated carcinogenic or non-carcinogenic health risks. While there was significant heterogeneity in the type of environmental substrate studied, collection method, and study design, the totality of results suggests significant environmental contamination across a variety of media poses a significant risk. Most studies reported calculated health risks above standard acceptable levels in at least one assay. While these studies do not measure health outcomes in human participants, environmental sampling can be used as a viable method of identifying populations that may be at risk of health effects from mining and should guide the development of future studies measuring direct health outcomes.
Limitations
Our study had several important limitations. First, our results are limited by the quality of studies included in our review; all data were observational, thus limiting the certainty of our findings. Types of bias likely introduced by this limitation include selection bias as well as reporting bias, with many consequences of mining going unreported. Second, our review was limited to articles available in English. Given the locations where mining typically occurs are low- and middle-income countries, there are likely many reports that were not captured in our search. Third, our review was limited to the PubMed database. Finally, while our search criteria were systematic in nature, the aim of this manuscript was not to conduct a systematic review of the literature. Our review was not prospectively registered and study quality and bias were not assessed. Therefore, for all of the above reasons, our results should be viewed as supportive of further research into this important field. The above limitations additionally reflect the current landscape of research into the hazards faced by miners. In that context, additional, comprehensive evaluation of the consequences inherent in such mining practices should be undertaken, and should aim to characterize additional key topics, such as the health effects of mining-related lithium toxicity and traumatic and infectious hazards associated with mining.
Conclusions
The information gathered in this narrative review strongly suggests that the global demand for LIBs and exponential growth of mining for cobalt, lithium, manganese, and nickel presents a significant risk to human health via occupational and environmental exposures that result in both acute and chronic toxicities. This is compounded by the facts that human rights violations are common in the mining industry and that the people most affected are often members of vulnerable populations, including children. Further research, particularly regarding the health and environmental effects of mining for lithium, is crucial to understanding and addressing the risks of the world’s growing reliance on LIBs.
Availability of data and materials
No datasets were generated or analyzed during the current study.
References
Harper G, et al. Recycling lithium-ion batteries from electric vehicles. Nature. 2019;575:75–86.
Research and Markets. Lithium-ion battery market, size, global forecast 2024–2028, Industry trends, share, growth, insight, impact of inflation, company analysis- product image lithium-ion battery market, size, global forecast 2024–2028, industry trends, share, growth, insight, impact of inflation, company analysis. https://www.researchandmarkets.com/reports/4790769/lithium-ion-battery-market-size-global?utm_source=GNE&utm_medium=PressRelease&utm_code=w89537&utm_campaign=1908598+-+Lithium-Ion+Battery+Market+to+Exceed+%24120+Billion+by+2028%3a+Electric+Vehicles+and+Renewable+Energy+Drive+Global+Expansion&utm_exec=jamu273prd#product--toc (2023).
Fleischmann, J. et al. Battery 2030: Resilient, sustainable, and circular. McKinsey & Company. https://www.mckinsey.com/industries/automotive-and-assembly/our-insights/battery-2030-resilient-sustainable-and-circular (2023).
Llamas-Orozco JA, et al. Estimating the environmental impacts of global lithium-ion battery supply chain: a temporal, geographical, and technological perspective. PNAS Nexus. 2023;2:pgad361.
Warner, J. T. Lithium-ion battery chemistries: a primer. Elsevier. 2019.
United States Department of Energy. Reducing reliance on cobalt for lithium-ion batteries. 2021. Energy.gov. https://www.energy.gov/eere/vehicles/articles/reducing-reliance-cobalt-lithium-ion-batteries.
Amnesty International. Democratic Republic of Congo: ‘This is what we die for’: Human rights abuses in the Democratic Republic of the Congo power the global trade in cobalt. Amnesty International https://www.amnesty.org/en/documents/afr62/3183/2016/en/.
Johanson P. Cobalt. New York; The Rosen Publishing Group, Inc. 2008.
Chen, R. J. & Lee, V. R. Cobalt toxicity. In StatPearls. Treasure Island: StatPearls Publishing; 2023.
Evans, G. & Masullo, L. Manganese toxicity. In StatPearls. Treasure Island: StatPearls Publishing; 2023.
Cameron KS, Buchner V, Tchounwou PB. Exploring the molecular mechanisms of nickel-induced genotoxicity and carcinogenicity: a literature review. 2011.
Gates, A., Jakubowski, J. A. & Regina, A. C. Nickel toxicology. In StatPearls. Treasure Island: StatPearls Publishing; 2023.
Hedya SA, Avula A, & Swoboda HD. Lithium toxicity. In StatPearls. StatPearls Publishing, 2023.
McKnight RF, et al. Lithium toxicity profile: a systematic review and meta-analysis. The Lancet. 2012;379:721–8.
Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–9.
Asante KA, et al. Contamination status of arsenic and other trace elements in drinking water and residents from Tarkwa, a historic mining township in Ghana. Chemosphere. 2007;66:1513–22.
Banza CL, et al. High human exposure to cobalt and other metals in Katanga, a mining area of the Democratic Republic of Congo. Env Res. 2009;109:745–52.
Banza Lubaba Nkulu C, et al. Sustainability of artisanal mining of cobalt in DR Congo. Nat Sustain. 2018;1:495–504.
Basu N, et al. A combined ecological and epidemiologic investigation of metal exposures amongst Indigenous peoples near the Marlin Mine in Western Guatemala. Sci Total Env. 2010;409:70–7.
Basu N, Nam DH, Kwansaa-Ansah E, Renne EP, Nriagu JO. Multiple metals exposure in a small-scale artisanal gold mining community. Env Res. 2011;111:463–7.
Cavalheiro Paulelli AC, et al. Fundão tailings dam failure in Brazil: Evidence of a population exposed to high levels of Al, As, Hg, and Ni after a human biomonitoring study. Env Res. 2022;205:112524.
Cheyns K, et al. Pathways of human exposure to cobalt in Katanga, a mining area of the D.R. Congo. Sci Total Env. 2014;490:313–21.
Henríquez-Hernández LA, et al. Pattern of blood concentrations of 47 elements in two populations from the same geographical area but with different geological origin and lifestyles: Canary Islands (Spain) vs. Morocco Sci Total Env. 2018;636:709–16.
Jefferson JA, et al. Excessive erythrocytosis, chronic mountain sickness, and serum cobalt levels. Lancet. 2002;359:407–8.
Kabamba Ngombe L, et al. Silicosis in underground miners in Lubumbashi, Democratic Republic of the Congo: 27 cases. Med Sante Trop. 2018;28:395–8.
Kayembe-Kitenge T, et al. Holoprosencephaly: A case series from an area with high mining-related pollution. Birth Defects Res. 2019;111:1561–3.
Kayembe-Kitenge T, et al. Agnathia otocephaly: A case from the Katanga Copperbelt. Birth Defects Res. 2020;112:1287–91.
Kayembe-Kitenge T, et al. Transplacental transfer of cobalt: Evidence from a study of mothers and their neonates in the African Copperbelt. J Trace Elem Med Biol. 2023;80:127294.
Mamuya S, Sakwari G, Ngowi V, Moen B, Bråtveit M. Dust Exposure, Fractional Exhaled Nitric Oxide and Respiratory Symptoms among Volcanic Rock Miners in Kilimanjaro. Tanzania Ann Glob Health. 2018;84:380–6.
Marsh GM, Esmen NA, Buchanich JM, Youk AO. Mortality patterns among workers exposed to arsenic, cadmium, and other substances in a copper smelter. Am J Ind Med. 2009;52:633–44.
Moreno ME, et al. Biomonitoring of metal in children living in a mine tailings zone in Southern Mexico: a pilot study. Int J Hyg Env Health. 2010;213:252–8.
Muimba-Kankolongo A, Banza Lubaba Nkulu C, Mwitwa J, Kampemba FM, Mulele Nabuyanda M. Impacts of Trace metals pollution of water, food crops, and ambient air on population health in Zambia and the DR Congo. J Env Public Health. 2022;2022:4515115.
Musa Obadia P, Kayembe-Kitenge T, Banza Lubaba Nkulu C, Enzlin P, Nemery B. Erectile dysfunction and mining-related jobs: an explorative study in Lubumbashi, Democratic Republic of Congo. Occup Env Med. 2020;77:19–21.
Musa Obadia P, et al. Erectile dysfunction in copper and cobalt miners: a cross-sectional study in the former Katanga province Democratic Republic of the Congo. Sex Med. 2023;11:qfad052.
Nakaona L, Maseka KK, Hamilton EM, Watts MJ. Using human hair and nails as biomarkers to assess exposure of potentially harmful elements to populations living near mine waste dumps. Env Geochem Health. 2020;42:1197–209.
Ndilila W, Callan AC, McGregor LA, Kalin RM, Hinwood AL. Environmental and toenail metals concentrations in copper mining and non mining communities in Zambia. Int J Hyg Env Health. 2014;217:62–9.
Nuvolone D, et al. Levels and determinants of urinary and blood metals in the geothermal area of Mt. Amiata in Tuscany (Italy). Env Sci Pollut Res Int. 2023;30:38319–32.
Semenova IN, Rafikova YS, Khasanova RF, Suyundukov YT. Analysis of metal content in soils near abandoned mines of Bashkir Trans-Urals and in the hair of children living in this territory. J Trace Elem Med Biol. 2018;50:664–70.
Sichletidis L, et al. The effect of environmental pollution on the respiratory system of lignite miners: a diachronic study. Med Lav. 2004;95:452–64.
Smolders E, et al. Unprecedentedly High Dust Ingestion Estimates for the General Population in a Mining District of DR Congo. Env Sci Technol. 2019;53:7851–8.
St-Jean A, et al. Nickel and associated metals in New Caledonia: exposure levels and their determinants. Env Int. 2018;118:106–15.
Tarabichi Y, Saggar R, Wallace WD, Lynch JP 3rd. Primary disease recurrence after single lung transplantation in a patient with prior hard metal exposure. J Heart Lung Transpl. 2015;34:1216–8.
Van Brusselen D, et al. Metal mining and birth defects: a case-control study in Lubumbashi, Democratic Republic of the Congo. Lancet Planet Health. 2020;4:e158–67.
Ayuso-Álvarez A, et al. Association between heavy metals and metalloids in topsoil and mental health in the adult population of Spain. Env Res. 2019;179:108784.
Badri H, Polya DA, Povey AC. Geochemical compositional controls on DNA strand breaks induced in in vitro cell-free assays by crushed rock powders from the Panasqueira mine area. Portugal Env Geochem Health. 2021;43:2631–47.
Betancourt Ó, Tapia M, Méndez I. Decline of general intelligence in children exposed to manganese from mining contamination in Puyango River Basin. Southern Ecuador Ecohealth. 2015;12:453–60.
Boojar MM, Goodarzi F. A longitudinal follow-up of pulmonary function and respiratory symptoms in workers exposed to manganese. J Occup Env Med. 2002;44:282–90.
Boojar MM, Goodarzi F, Basedaghat MA. Long-term follow-up of workplace and well water manganese effects on iron status indexes in manganese miners. Arch Env Health. 2002;57:519–28.
Catalán-Vázquez M, Schilmann A, Riojas-Rodríguez H. Perceived health risks of manganese in the Molango Mining District. Mexico Risk Anal. 2010;30:619–34.
Catalán-Vázquez M, Riojas-Rodríguez H, Pelcastre-Villafuerte BE. Risk perception and social participation among women exposed to manganese in the mining district of the state of Hidalgo. Mexico Sci Total Env. 2012;414:43–52.
Catalán-Vázquez M, Riojas-Rodríguez H, Pelcastre-Villafuerte BE. Risk: for whom? representations of mining activity by different social actors in the Molango Manganese District of Hidalgo. Mexico Risk Anal. 2014;34:28–43.
Catalán-Vázquez M, Riojas-Rodríguez H. Gender inequity in health in contexts of environmental risk from mining and industrial activity in Mexico. Rev Panam Salud Publica. 2015;37:379–87.
Claus Henn B, et al. Prenatal arsenic exposure and birth outcomes among a population residing near a mining-related superfund site. Env Health Perspect. 2016;124:1308–15.
Claus Henn B, et al. Maternal and cord blood manganese concentrations and early childhood neurodevelopment among residents near a mining-impacted superfund site. Env Health Perspect. 2017;125:067020.
Coelho P, et al. Metal(loid) levels in biological matrices from human populations exposed to mining contamination–Panasqueira Mine (Portugal). J Toxicol Env Health A. 2012;75:893–908.
Coelho P, et al. Genotoxic effect of exposure to metal(loid)s. A molecular epidemiology survey of populations living and working in Panasqueira mine area, Portugal. Env Int. 2013;60:163–70.
Cortez-Lugo M, et al. Evaluation of the effect of an environmental management program on exposure to manganese in a mining zone in Mexico. Neurotoxicology. 2018;64:142–51.
Cortez-Lugo M, et al. Neurocognitive function in adult residents of a mining district in Mexico after reducing manganese exposure: Follow-up after 11 years. Sci Total Env. 2022;848:157519.
Criswell SR, et al. Ex vivo magnetic resonance imaging in South African manganese mine workers. Neurotoxicology. 2015;49:8–14.
Dai L, et al. Potentially toxic elements in human scalp hair around China’s largest polymetallic rare earth ore mining and smelting area. Env Int. 2023;172:107775.
Dlamini WW, Nelson G, Nielsen SS, Racette BA. Manganese exposure, parkinsonian signs, and quality of life in South African mine workers. Am J Ind Med. 2020;63:36–43.
Duka YD, Ilchenko SI, Kharytonov MM, Vasylyeva TL. Impact of open manganese mines on the health of children dwelling in the surrounding area. Emerg Health Threats J. 2011;4:7110.
García-Chimalpopoca Z, et al. Verbal memory and learning in schoolchildren exposed to manganese in Mexico. Neurotox Res. 2019;36:827–35.
Gonzalez-Cuyar LF, et al. Quantitative neuropathology associated with chronic manganese exposure in South African mine workers. Neurotoxicology. 2014;45:260–6.
González-Merizalde MV, et al. Manganese and mercury levels in water, sediments, and children living near gold-mining areas of the Nangaritza River Basin. Ecuadorian Amazon Arch Env Contam Toxicol. 2016;71:171–82.
Hernández-Bonilla D, et al. Effects of manganese exposure on visuoperception and visual memory in schoolchildren. Neurotoxicology. 2016;57:230–40.
Hinwood A, Callan AC, Heyworth J, McCafferty P, Sly PD. Children’s personal exposure to PM10 and associated metals in urban, rural and mining activity areas. Chemosphere. 2014;108:125–33.
Hochberg F, et al. Late motor deficits of Chilean manganese miners: a blinded control study. Neurology. 1996;47:788–95.
Hoover JH, et al. Exposure to uranium and co-occurring metals among pregnant Navajo women. Env Res. 2020;190:109943.
Huang Y, Bao M, Xiao J, Qiu Z, & Wu K. Effects of PM(2.5) on cardio-pulmonary function injury in open manganese mine workers. Int J Env. Res Public Health 2019;16:2017.
Kissani N, Naji Y, Mebrouk Y, Chraa M, Ghanima A. Parkinsonism and chronic manganese exposure: pilot study with clinical, environmental and experimental evidence. Clin Park Relat Disord. 2020;3:100057.
Lopes de Andrade V, et al. Multibiomarker approach to assess the magnitude of occupational exposure and effects induced by a mixture of metals. Toxicol Appl Pharmacol. 2021;429:115684.
Lourenço J, et al. Biomonitoring a human population inhabiting nearby a deactivated uranium mine. Toxicology. 2013;305:89–98.
Molina-Villalba I, et al. Biomonitoring of arsenic, cadmium, lead, manganese and mercury in urine and hair of children living near mining and industrial areas. Chemosphere. 2015;124:83–91.
Mortazavi S, Mortazavi G, Paknahad M. Levels of arsenic, mercury, cadmium, copper, lead, zinc, and manganese in serum and whole blood of resident adults from mining and non-mining communities in Ghana. Env Sci Pollut Res Int. 2016;23:22220–1.
Mota PJ, et al. Prevalence of metal levels above the reference values in a municipality affected by the collapse of a mining tailings dam: Brumadinho Health Project. Rev Bras Epidemiol. 2022;25:e220014.
Motas M, Jiménez S, Oliva J, Cámara MÁ, & Pérez-Cárceles MD. Heavy metals and trace elements in human breast milk from industrial/mining and agricultural zones of southeastern Spain. Int J Env Res Public Health. 2021;18:9289.
Myers JE, et al. Nervous system effects of occupational manganese exposure on South African manganese mineworkers. Neurotoxicology. 2003;24:649–56.
Myers JE, et al. The utility of biological monitoring for manganese in ferroalloy smelter workers in South Africa. Neurotoxicology. 2003;24:875–83.
Myers JE, et al. The nervous system effects of occupational exposure on workers in a South African manganese smelter. Neurotoxicology. 2003;24:885–94.
Nakata S, Sato J, Imai K, Yamanaka H, Ichinose Y. Epidemiological characteristics of prostate cancer in Gunma Prefecture, Japan. Gunma University Urological Oncology study group. Int J Urol. 1995;2:191–7.
Nelson G, Criswell SR, Zhang J, Murray J, Racette BA. Research capacity development in South African manganese mines to bridge exposure and neuropathologic outcomes. Neurotoxicology. 2012;33:683–6.
Nyanza EC, Joseph M, Premji SS, Thomas DS, Mannion C. Geophagy practices and the content of chemical elements in the soil eaten by pregnant women in artisanal and small scale gold mining communities in Tanzania. BMC Pregnancy Childbirth. 2014;14:144.
Obiri S, Yeboah PO, Osae S, Adu-Kumi S. Levels of arsenic, mercury, cadmium, copper, lead, zinc and manganese in serum and whole blood of resident adults from mining and non-mining communities in Ghana. Env Sci Pollut Res Int. 2016;23:16589–97.
Parente CET, et al. First assessment of atmospheric pollution by trace elements and particulate matter after a severe collapse of a tailings dam, Minas Gerais, Brazil: an insight into biomonitoring with Tillandsia usneoides and a public health dataset. Env Res. 2023;233:116435.
Pelders J, Nelson G. Socio-demographic contributors to health and safety of mine workers in South Africa. Work. 2019;64:67–76.
Reutova NV, Reutova TV, Dreeva FR, Shevchenko AA. Long-term impact of the Tyrnyauz tungsten-molybdenum mining and processing factory waste on environmental pollution and children’s population. Env Geochem Health. 2022. https://doi.org/10.1007/s10653-022-01221-z.
Riojas-Rodríguez H, et al. Intellectual function in Mexican children living in a mining area and environmentally exposed to manganese. Env Health Perspect. 2010;118:1465–70.
Rodier J. Manganese poisoning in Moroccan miners. Br J Ind Med. 1955;12:21.
Santos-Burgoa C, et al. Exposure to manganese: health effects on the general population, a pilot study in central Mexico. Env Res. 2001;85:90–104.
Saunders JE, et al. Hearing loss and heavy metal toxicity in a Nicaraguan mining community: audiological results and case reports. Audiol Neurootol. 2013;18:101–13.
Schuler P, et al. Manganese poisoning. Environmental and medical study at a Chilean mine. Ind Med Surg. 1957;26:167–73.
Serrazina DC, et al. Biomarkers of exposure and effect in a working population exposed to lead, manganese and arsenic. J Toxicol Env Health A. 2018;81:983–97.
Sweet DV, Crouse WE, Crable JV, Carlberg JR, Lainhart WS. The relationship of total dust, free silica, and trace metal concentrations to the occupational respiratory disease of bituminous coal miners. Am Ind Hyg Assoc J. 1974;35:479–88.
Verma S, Chaudhari S. Safety of workers in indian mines: study, analysis, and prediction. Saf Health Work. 2017;8:267–75.
Vinayagamoorthy N, et al. Genetic polymorphism of CYP2D6∗2 C→T 2850, GSTM1, NQO1 genes and their correlation with biomarkers in manganese miners of Central India. Chemosphere. 2010;81:1286–91.
Vormittag E, Saldiva P, Anastacio A, Barbosa F Jr. High levels of metals/metalloids in blood and urine of residents living in the area affected by the dam failing in Barra Longa, District, Brazil: a preliminary human biomonitoring study. Env Toxicol Pharmacol. 2021;83:103566.
Wang J, et al. Identification of Histoplasma causing an unexplained disease cluster in Matthews Ridge. Guyana Biosaf Health. 2019;1:150–4.
Watanabe H, Mishina T, Ohe H, Araki H, Nakao M. A clustering of prostatic cancer in an area with many manganese mines. Tohoku J Exp Med. 1981;135:441–2.
Zhou L, et al. An Outbreak of Febrile Histoplasmosis Among Chinese Manganese-Mine Workers in Cooperative Republic of Guyana in 2019. China CDC Wkly. 2019;1:38–42.
Zota AR, et al. Associations between metals in residential environmental media and exposure biomarkers over time in infants living near a mining-impacted site. J Expo Sci Env Epidemiol. 2016;26:510–9.
Zhumalina AK, Bekmukhambetov EZ, Tusupkaliev BT, Zharlikasinova MB. Development of scientifically justified proposals on the prevention and treatment of environmentally determined constitutional growth delay in children in the West Kazakhstan region. Env Geochem Health. 2019;41:1251–65.
Aguilera I, et al. Urinary levels of arsenic and heavy metals in children and adolescents living in the industrialised area of Ria of Huelva (SW Spain). Env Int. 2010;36:563–9.
Berriault CJ, Lightfoot NE, Seilkop SK, Conard BR. Injury mortality in a cohort of mining, smelting, and refining workers in Ontario. Arch Env Occup Health. 2017;72:220–30.
Cavalheiro Paulelli AC, et al. Association between urinary concentrations of toxic metals/metalloids and oxidative stress in Brazilians living in areas affected by the Fundão dam failure. Env Res. 2023;238:117307.
Cocco P, et al. Lung cancer risk, silica exposure, and silicosis in Chinese mines and pottery factories: the modifying role of other workplace lung carcinogens. Am J Ind Med. 2001;40:674–82.
Cortés S, Lagos LDCM, Burgos S, Adaros H, Ferreccio C. Urinary metal levels in a Chilean community 31 years after the dumping of mine tailings. J Health Pollut. 2016;6:19–27.
Cortés S et al. A Positive relationship between exposure to heavy metals and development of chronic diseases: a case study from Chile. Int J Env Res Public Health. 2021;18:1419.
Ekosse G. General health status of residents of the Selebi Phikwe Ni-Cu mine area. Botswana Int J Env Health Res. 2005;15:373–81.
Ekosse G, de Jager L, van den Heever DJ. The occurrences of chest pains and frequent coughing among residents living within the Selebi Phikwe Ni-Cu mine area. Botswana Afr J Health Sci. 2005;12:37–48.
Ekosse GI. Health status within the precincts of a nickel-copper mining and smelting environment. Afr Health Sci. 2011;11:90–6.
Erdei E, et al. Metal mixture exposures and multiplexed autoantibody screening in Navajo communities exposed to uranium mine wastes. J Transl Autoimmun. 2023;6:100201.
Goldberg M, et al. Epidemiology of respiratory cancers related to nickel mining and refining in New Caledonia (1978–1984). Int J Cancer. 1987;40:300–4.
Goldberg M, et al. A 10-year incidence survey of respiratory cancer and a case-control study within a cohort of nickel mining and refining workers in New Caledonia. Cancer Causes Control. 1994;5:15–25.
Hopfer SM, Fay WP, Sunderman FW Jr. Serum nickel concentrations in hemodialysis patients with environmental exposure. Ann Clin Lab Sci. 1989;19:161–7.
Khlifi R, et al. Biomonitoring of cadmium, chromium, nickel and arsenic in general population living near mining and active industrial areas in Southern Tunisia. Env Monit Assess. 2014;186:761–79.
Kramer DM, et al. From awareness to action: Sudbury, mining and occupational disease in a time of change. Work. 2017;58:149–62.
Kusiak RA, Springer J, Ritchie AC, Muller J. Carcinoma of the lung in Ontario gold miners: possible aetiological factors. Br J Ind Med. 1991;48:808–17.
Leclerc A, Goldberg M, Goldberg P, Deloumeaux J, Fuhrer R. Geographical distribution of respiratory cancer in New Caledonia. Arch Env Health. 1987;42:315–20.
Lightfoot NE, Berriault CJ, Seilkop SK, Conard BR. Nonrespiratory mortality and cancer incidence in a cohort of Canadian nickel workers. Arch Env Occup Health. 2017;72:187–203.
Li Y, Sun X, Ge H, Liu J, & Chen L. The status of occupational stress and its influence the quality of life of copper-nickel miners in Xinjiang, China. Int J Env Res Public Health. 2019;16:353.
Miranda-Guevara A, et al. The dangerous link between coal dust exposure and DNA damage: unraveling the role of some of the chemical agents and oxidative stress. Env Geochem Health. 2023;45:7081–97.
Nieminen P et al. Environmental exposure as an independent risk factor of chronic bronchitis in northwest Russia. Int J Circumpolar Health. 2013;72:19742.
Nordin AP, et al. In vitro genotoxic effect of secondary minerals crystallized in rocks from coal mine drainage. J Hazard Mater. 2018;346:263–72.
Norseth T. Environmental pollution around nickel smelters in the Kola Peninsula (Russia). Sci Total Env. 1994;148:103–8.
Seilkop SK, Lightfoot NE, Berriault CJ, Conard BR. Respiratory cancer mortality and incidence in an updated cohort of Canadian nickel production workers. Arch Env Occup Health. 2017;72:204–19.
Shannon HS, Julian JA, Roberts RS. A mortality study of 11,500 nickel workers. J Natl Cancer Inst. 1984;73:1251–8.
Shannon HS, et al. Mortality of 11,500 nickel workers–extended follow up and relationship to environmental conditions. Toxicol Ind Health. 1991;7:277–94.
Smith-Sivertsen T, et al. Sulphur dioxide exposure and lung function in a Norwegian and Russian population living close to a nickel smelter. Int J Circumpolar Health. 2001;60:342–59.
Sun X, Zhang L, Zhang C, Liu J, Ge H. The status of job burnout and its influence on the working ability of copper-nickel miners in Xinjiang. China BMC Public Health. 2020;20:305.
Tasnim T & Sunarsih. Analysis of impaired kidney function in the community around the Morosi nickel mines. J Public Health Afr. 2023;14:2700.
Taylor MP. Atmospherically deposited trace metals from bulk mineral concentrate port operations. Sci Total Env. 2015;515–516:143–52.
Verma DK, et al. Polycyclic aromatic hydrocarbons (PAHs): a possible cause of lung cancer mortality among nickel/copper smelter and refinery workers. Am Ind Hyg Assoc J. 1992;53:317–24.
Verma DK. Metals in the lungs of Ontario hardrock miners. Arch Env Occup Health. 2013;68:180–3.
Wang X, et al. Metal Biomonitoring and Comparative Assessment in Urine of Workers in Lead-Zinc and Steel-Iron Mining and Smelting. Biol Trace Elem Res. 2019;189:1–9.
Yang AM, et al. Metal exposure and risk of diabetes and prediabetes among Chinese occupational workers. Biomed Env Sci. 2015;28:875–83.
Zhang WC, Zhang QF, Song ZF. Studies on the hazardous effects and the maximum allowable concentration of pyrophyllite dust. Biomed Env Sci. 1997;10:377–86.
Amponsah-Tawiah K, Jain A, Leka S, Hollis D, Cox T. Examining psychosocial and physical hazards in the Ghanaian mining industry and their implications for employees’ safety experience. J Safety Res. 2013;45:75–84.
Adjei-Mensah R, et al. Effect of home processing methods on the levels of heavy metal contaminants in four food crops grown in and around two mining towns in Ghana. Toxicol Rep. 2021;8:1830–8.
Aendo P, et al. Health significant alarms of toxic carcinogenic risk consumption of blood meal metals contamination in poultry at a gold mining neighborhood, northern Thailand. Env Geochem Health. 2022;44:783–97.
Akoto O, et al. Characterization, spatial variation and risk assessment of heavy metals and a metalloid in surface soils in Obuasi. Ghana J Health Pollut. 2018;8:180902.
Al-Swadi HA, et al. Sources, toxicity potential, and human health risk assessment of heavy metals-laden soil and dust of urban and suburban areas as affected by industrial and mining activities. Sci Rep. 2022;12:8972.
Antoniadis V, et al. Bioavailability and risk assessment of potentially toxic elements in garden edible vegetables and soils around a highly contaminated former mining area in Germany. J Env Manage. 2017;186:192–200.
Antunović V, Blagojević D, Baošić R, Relić D, Lolić A. Health risk assessment of heavy metals in soil, plant, and water samples near ‘Gacko’ power plant, in Bosnia and Herzegovina. Env Monit Assess. 2023;195:596.
Barjoee SS, Abadi SZM, Elmi MR, Varaoon VT, Nikbakht M. Evaluation of trace elements pollution in deposited dust on residential areas and agricultural lands around Pb/Zn mineral areas using modified pollution indices. J Env Health Sci Eng. 2021;19:753–69.
Bartrem C, et al. Unknown risk: co-exposure to lead and other heavy metals among children living in small-scale mining communities in Zamfara State. Nigeria Int J Env Health Res. 2014;24:304–19.
Canpolat Ö, Varol M, Okan ÖÖ, Eriş KK. Sediment contamination by trace elements and the associated ecological and health risk assessment: a case study from a large reservoir (Turkey). Env Res. 2022;204:112145.
Chai Y & Guo F. Potentially toxic element contamination in soils affected by the antimony mine spill in northwest China. Toxics. 2023;11:359.
Chan WS, et al. Metal accumulations in aquatic organisms and health risks in an acid mine-affected site in South China. Env Geochem Health. 2021;43:4415–40.
Chen F, et al. Evaluation of toxicity potential of cobalt in wheat irrigated with wastewater: health risk implications for public. Env Sci Pollut Res Int. 2021;28:21119–31.
Cheng X, et al. Characteristics, Sources and Health Risk Assessment of Trace Metals in PM(10) in Panzhihua. China Bull Env Contam Toxicol. 2017;98:76–83.
Cheng J, Zhang X, Ren S, Wang T, Tang Z. Metals in wild fish from Gaotang Lake in the area of coal mining, China: assessment of the risk to human health. Env Sci Pollut Res Int. 2019;26:23754–62.
Chris DI, Onyena AP, Sam K. Evaluation of human health and ecological risk of heavy metals in water, sediment and shellfishes in typical artisanal oil mining areas of Nigeria. Env Sci Pollut Res Int. 2023;30:80055–69.
Chu Z, et al. Lability, bioaccessibility, and ecological and health risks of anthropogenic toxic heavy metals in the arid calcareous soil around a nonferrous metal smelting area. Chemosphere. 2022;307:136200.
Compaore WF, Dumoulin A, Rousseau DPL. Trace element content in cereals from a gold mining site in Burkina Faso and intake risk assessment. J Env Manage. 2019;248:109292.
Correia L, et al. Bioaccumulation of nickel in tomato plants: risks to human health and agro-environmental impacts. Env Monit Assess. 2018;190:317.
Darko G, et al. Human health risk and bioaccessibility of toxic metals in topsoils from Gbani mining community in Ghana. J Health Pollut. 2019;9:190602.
Du Y, et al. Different exposure profile of heavy metal and health risk between residents near a Pb-Zn mine and a Mn mine in Huayuan county. South China Chemosphere. 2019;216:352–64.
Fan Y, Zhu T, Li M, He J, Huang R. Heavy metal contamination in soil and brown rice and human health risk assessment near three mining areas in central China. J Heal Eng. 2017;2017:4124302.
Focus E, Rwiza MJ, Mohammed NK, Banzi FP. Health risk assessment of trace elements in soil for people living and working in a mining area. J Env Public Health. 2021;2021:9976048.
Genthe B, et al. Health risk implications from simultaneous exposure to multiple environmental contaminants. Ecotoxicol Env Saf. 2013;93:171–9.
Hao H, Li P, Lv Y, Chen W, Ge D. Probabilistic health risk assessment for residents exposed to potentially toxic elements near typical mining areas in China. Env Sci Pollut Res Int. 2022;29:58791–809.
Hasimuna OJ, et al. Contamination of selected heavy metals in Limnothrissa miodon (Boulenger, 1906) in the four strata of Lake Kariba Zambia: are the consumers at risk? J Env Sci Health B. 2023;58:521–9.
Jia Y, Wang L, Cao J, Li S, Yang Z. Trace elements in four freshwater fish from a mine-impacted river: spatial distribution, species-specific accumulation, and risk assessment. Env Sci Pollut Res Int. 2018;25:8861–70.
Ju Q, et al. Source apportionment and ecological health risks assessment from major ions, metalloids and trace elements in multi-aquifer groundwater near the Sunan mine area. Eastern China Sci Total Env. 2023;860:160454.
Kamunda C, Mathuthu M, & Madhuku M. Health risk assessment of heavy metals in soils from Witwatersrand gold mining basin, South Africa. Int J Env Res Public Health. 2016;13:663.
Kazemi A, Esmaeilbeigi M, Sahebi Z, Shooshtari SJ. Hydrochemical evaluation of groundwater quality and human health risk assessment of trace elements in the largest mining district of South Khorasan, Eastern Iran. Env Sci Pollut Res Int. 2022;29:81804–29.
Khan ZI, et al. A study on the seasonal transfer of two metals from pasture to animals: health risk assessment. Env Sci Pollut Res Int. 2020;27:16339–49.
Kurilić SM, Božilović Z, Milošević R. Contamination and health risk assessment of trace elements in PM(10) from mining and smelting operations in the Bor Basin. Serbia Toxicol Ind Health. 2020;36:135–45.
Le TT, Kim KW, Nguyen DQ, Ngo HTT. Trace element contamination in rice and its potential health risks to consumers in North-Central Vietnam. Env Geochem Health. 2022. https://doi.org/10.1007/s10653-022-01415-5.
Li H, et al. Distribution of heavy metals and metalloids in bulk and particle size fractions of soils from coal-mine brownfield and implications on human health. Chemosphere. 2017;172:505–15.
Li H, et al. Quantifying ecological and human health risks of metal(loid)s pollution from non-ferrous metal mining and smelting activities in Southwest China. Sci Total Env. 2023;873:162364.
Liu K, et al. Concentrations and health risks of heavy metals in soils and crops around the Pingle manganese (Mn) mine area in Guangxi Province. China Env Sci Pollut Res Int. 2018;25:30180–90.
Liu H, et al. Heavy metal accumulation in the surrounding areas affected by mining in China: spatial distribution patterns, risk assessment, and influencing factors. Sci Total Env. 2022;825:154004.
Long J, Luo K. Elements in surface and well water from the central North China Plain: enrichment patterns, origins, and health risk assessment. Env Pollut. 2020;258:113725.
Luo L, et al. Phytoavailability, bioaccumulation, and human health risks of metal(loid) elements in an agroecosystem near a lead-zinc mine. Env Sci Pollut Res Int. 2018;25:24111–24.
Luo X, Ren B, Hursthouse AS, Jiang F, Deng RJ. Potentially toxic elements (PTEs) in crops, soil, and water near Xiangtan manganese mine, China: potential risk to health in the foodchain. Env Geochem Health. 2020;42:1965–76.
Luo X, Ren B, Hursthouse AS, Thacker JRM, & Wang Z. Soil from an Abandoned manganese mining area (Hunan, China): significance of health risk from potentially toxic element pollution and its spatial context. Int J Env Res Public Health. 2020;17:6554.
Mafulul SG, Joel EB, Gushit J. Health risk assessment of potentially toxic elements (PTEs) concentrations in soil and fruits of selected perennial economic trees growing naturally in the vicinity of the abandoned mining ponds in Kuba, Bokkos Local Government Area (LGA) Plateau State. N Env Geochem Health. 2023;45:5893–914.
Malik N, Elumalai SP, Kumar K. Health risk assessment from exposure to ambient VOCs and particulate matter in different functional zones in Dhanbad. India Sci Total Env. 2023;891:164573.
Mehta N, et al. Extractive waste management: a risk analysis approach. Sci Total Env. 2018;622–623:900–12.
Mwelwa S, Chungu D, Tailoka F, Beesigamukama D, Tanga C. Biotransfer of heavy metals along the soil-plant-edible insect-human food chain in Africa. Sci Total Env. 2023;881:163150.
Neris JB, et al. HERisk: An improved spatio-temporal human health risks assessment software. Sci Total Env. 2021;772:145044.
Neves MO, Figueiredo VR, Abreu MM. Transfer of U, Al and Mn in the water-soil-plant (Solanum tuberosum L.) system near a former uranium mining area (Cunha Baixa, Portugal) and implications to human health. Sci Total Env. 2012;416:156–63.
Ngole-Jeme VM, Fantke P. Ecological and human health risks associated with abandoned gold mine tailings contaminated soil. PLoS ONE. 2017;12: e0172517.
Orisakwe OE, Oladipo OO, Ajaezi GC, Udowelle NA. Horizontal and Vertical Distribution of Heavy Metals in Farm Produce and Livestock around Lead-Contaminated Goldmine in Dareta and Abare, Zamfara State. Northern Nigeria J Env Public Health. 2017;2017:3506949.
Orisakwe OE, Dagur EA, Mbagwu HOC, Udowelle NA, Offor SJ. Levels of some heavy metals in vegetables from artisanal mining sites of Dilimi River, Bukuru and Barkin Ladi North Central Nigeria: any public health concern? Rocz Panstw Zakl Hig. 2018;69:335–45.
Pavilonis B, Grassman J, Johnson G, Diaz Y, Caravanos J. Characterization and risk of exposure to elements from artisanal gold mining operations in the Bolivian Andes. Env Res. 2017;154:1–9.
Pipoyan D, Beglaryan M, Stepanyan S, Merendino N. Dietary exposure assessment of potentially toxic trace elements in fruits and vegetables sold in town of Kapan. Armenia Biol Trace Elem Res. 2019;190:234–41.
Rehman IU, et al. Enrichment, spatial distribution of potential ecological and human health risk assessment via toxic metals in soil and surface water ingestion in the vicinity of Sewakht mines, district Chitral. Northern Pakistan Ecotoxicol Env Saf. 2018;154:127–36.
Rodriguez-Levy IE, Van Damme PA, Carvajal-Vallejos FM, Bervoets L. Trace element accumulation in different edible fish species from the Bolivian Amazon and the risk for human consumption. Heliyon. 2022;8: e11649.
Romero-Crespo P, et al. Trace elements in farmland soils and crops, and probabilistic health risk assessment in areas influenced by mining activity in Ecuador. Env Geochem Health. 2023;45:4549–63.
Sangaré LO, Ba S, Diallo O, Sanogo D, Zheng T. Assessment of potential health risks from heavy metal pollution of surface water for drinking in a multi-industry area in Mali using a multi-indices approach. Env Monit Assess. 2023;195:700.
Shi X, Ren B, Hursthouse A. Source identification and groundwater health risk assessment of PTEs in the stormwater runoff in an abandoned mining area. Env Geochem Health. 2022;44:3555–70.
Shi J, Zhao D, Ren F, Huang L. Spatiotemporal variation of soil heavy metals in China: the pollution status and risk assessment. Sci Total Env. 2023;871:161768.
Souffit GD, Mohamadou LL, Guembou Shouop CJ, Beyala Ateba JF, & Saïdou-. Assessment of trace elements pollution and their potential health risks in the cobalt-nickel bearing areas of Lomié, East Cameroon. Env Monit Assess. 2022;194:127.
Yang Q, Chen H, Li B. Source identification and health risk assessment of metals in indoor dust in the vicinity of phosphorus mining, Guizhou Province. China Arch Env Contam Toxicol. 2015;68:20–30.
Zainab N, et al. Health risk assessment and bioaccumulation of potentially toxic metals from water, soil, and forages near coal mines of district Chakwal, Punjab. Pakistan Env Geochem Health. 2023;45:5441–66.
Zhao R, et al. Fuzzy synthetic evaluation and health risk assessment quantification of heavy metals in Zhangye agricultural soil from the perspective of sources. Sci Total Env. 2019;697:134126.
Harari F, et al. Environmental exposure to lithium during pregnancy and fetal size: a longitudinal study in the Argentinean Andes. Environ Int. 2015;77:48–54.
Memon A, et al. Association between naturally occurring lithium in drinking water and suicide rates: systematic review and meta-analysis of ecological studies. Br J Psychiatry. 2020;217:667–78.
Parker WF, et al. Association between groundwater lithium and the diagnosis of bipolar disorder and dementia in the United States. JAMA Psychiat. 2018;75:751–4.
Gao J-Q, et al. Effects of lithium resource exploitation on surface water at Jiajika mine. China Environ Monit Assess. 2021;193:1–16.
Vera ML, Torres WR, Galli CI, Chagnes A, Flexer V. Environmental impact of direct lithium extraction from brines. Nat Rev Earth Environ. 2023;4:149–65.
Denyer S. Tibetans in anguish as Chinese mines pollute their sacred grasslands. Washington, D.C.: Washington Post; 2016.
Shanks GD. Historical gold mining infectious disease epidemics. Intern Med J. 2022;52:1441–5.
Bausch DG, et al. Risk factors for Marburg hemorrhagic fever, Democratic Republic of the Congo. Emerg Infect Dis. 2003;9:1531.
Kelly J, Greenberg N, Sabet D & Fulp J. Assessment of Human trafficking in artisanal mining towns in Eastern Democratic Republic of the Cong. Wash. DC US Agency Int. Dev. 2014. https://pdf.usaid.gov/pdf_docs/PA00K5R1.pdf.
Steele S. Human trafficking, labor brokering, and mining in southern Africa: Responding to a decentralized and hidden public health disaster. Int J Health Serv. 2013;43:665–80.
Debela MB, Azage M, Begosaw AM, Kabeta ND. Factors contributing to occupational injuries among workers in the construction, manufacturing, and mining industries in Africa: a systematic review and meta-analysis. J Public Health Policy. 2022;43:487–502.
Allan-Blitz L-T, Goldfine C, Erickson TB. Environmental and health risks posed to children by artisanal gold mining: a systematic review. SAGE Open Med. 2022;10:20503121221076936.
Heng YY, et al. Heavy metals and neurodevelopment of children in low and middle-income countries: A systematic review. PLoS ONE. 2022;17: e0265536.
Al Osman M, Yang F, Massey IY. Exposure routes and health effects of heavy metals on children. Biometals. 2019;32:563–73.
Acknowledgements
Figure 1 was generated by Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Figure 2 was generated at www.mapchart.net.
Funding
We received no funding for this study.
Author information
Authors and Affiliations
Contributions
CB wrote the main manuscript text and prepared all figures. All authors contributed to article review for inclusion and approved the final manuscript text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not obtained given this study is a review of previously published work and does not include human or animal participants
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Brown, C.W., Goldfine, C.E., Allan-Blitz, LT. et al. Occupational, environmental, and toxicological health risks of mining metals for lithium-ion batteries: a narrative review of the Pubmed database. J Occup Med Toxicol 19, 35 (2024). https://doi.org/10.1186/s12995-024-00433-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12995-024-00433-6